글로벌 연구동향
방사선종양학
- 2023년 07월호
[J Gynecol Oncol .] Risk factors for lower extremity lymphedema after surgery in cervical and endometrial cancer
자궁경부암과 자궁내막암에서 수술후 하지 림프부종 위험요인연세의대 / 이준교, 김용배*
- 출처
- J Gynecol Oncol .
- 등재일
- 2023 May
- 저널이슈번호
- 34(3):e28. doi: 10.3802/jgo.2023.34.e28. Epub 2022 Dec 19.
- 내용
Abstract
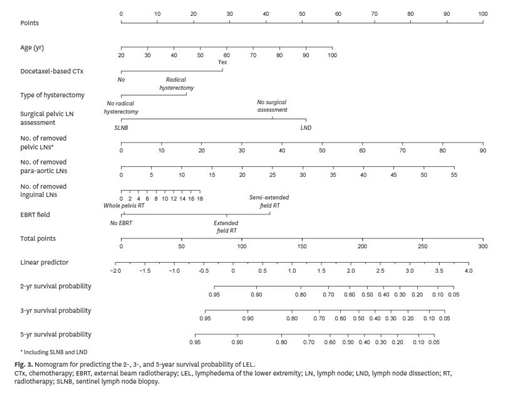
Objective: Lower extremity lymphedema (LEL) is a well-known adverse effect related to cervical and endometrial cancer (CEC); however, very few studies have elucidated the clinicopathologic risk factors related to LEL. We investigated the incidence and risk factors in patients who received primary surgery and/or adjuvant radiotherapy (RT) or chemotherapy for CEC.Methods: We retrospectively reviewed 2,565 patients who underwent primary surgery following CEC diagnosis between January 2007 and December 2020. LEL diagnosis was based on objective and subjective assessments by experts. We identified important predictors of LEL to construct a nomogram predicting individual risks of LEL. For internal validation of the nomogram, the original data were separated using the split-sample method in a 7:3 ratio of training data and test data.
Results: Overall, 858 patients (33.5%) received RT, 586 received external beam RT (EBRT), and 630 received intracavitary RT. During follow-up period, LEL developed in 331 patients, with an overall cumulative 5-year incidence of 13.3%. In multivariate analysis, age at primary treatment, use of docetaxel-based chemotherapy, type of hysterectomy, type of surgical pelvic lymph node (LN) assessment, number of dissected pelvic and para-aortic LNs, and EBRT field were the independent predictors of LEL. We subsequently developed the nomogram showing excellent predictive power for LEL.
Conclusion: LEL is associated with various treatment modalities, and their interactions may increase the possibility of occurrences. De-escalation strategies for treatment modalities should be considered to reduce LEL in patients with CEC.
Affiliations
Joongyo Lee 1, Hwa Kyung Byun 1, Sang Hee Im 2, Won Jeong Son 3, Yun Ho Roh 3, Yong Bae Kim 4
1Department of Radiation Oncology, Yonsei Cancer Center, Heavy Ion Therapy Research Institute, Yonsei University College of Medicine, Seoul, Korea.
2Department of Rehabilitation Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
3Biostatistics Collaboration Unit, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea.
4Department of Radiation Oncology, Yonsei Cancer Center, Heavy Ion Therapy Research Institute, Yonsei University College of Medicine, Seoul, Korea. ybkim3@yuhs.ac.
- 키워드
- Cervical Cancer; Endometrial Cancer; Lymphedema; Radiotherapy; Risk Factor.
- 덧글달기
- 이전글 [Clin Transl Radiat Oncol .] Vertebral compression fracture after stereotactic ablative radiotherapy in patients with oligometastatic bone lesions from hepatocellular carcinoma
- 다음글 [Int Wound J .] Early outcomes of complete excision followed by immediate postoperative single fractional 10 Gy for anterior chest keloids: A preliminary results








편집위원
부인암의 수술후 하지림프종 발생은 삶의 질을 심각하게 저하시키는 부작용으로, 후향적 연구를 통해 그 위험인자를 다양하게 제시했음. 특히 nomogram을 통한 하지림프종 발생 위험을 예측할 수 있다는 것과, 보조적 방사선치료 여부 및 방사선치료범위에 따라 하지림프종 위험이 달라질 수 있다는 것을 토대로 환자 맞춤형 방사선치료를 시행할 것을 권고한 점이 흥미로운 부분임.
덧글달기닫기2023-07-04 14:52:50
등록