글로벌 연구동향
방사선종양학
- [Clin Transl Radiat Oncol .] Incorporating axillary-lateral thoracic vessel juncture dosimetric variables improves model for predicting lymphedema in patients with breast cancer: A validation analysis
연세의대, 이화의대 / 장지석*, 고희주, 김규보*
- 출처
- Clin Transl Radiat Oncol .
- 등재일
- 2023 Apr 20
- 저널이슈번호
- 41:100629.
- 내용
Abstract
Background: A relationship between the axillary-lateral thoracic vessel juncture (ALTJ) dose and lymphedema rate has been reported in patients with breast cancer. The purpose of this study was to validate this relationship and explore whether incorporation of the ALTJ dose-distribution parameters improves the prediction model's accuracy.Methods: A total of 1,449 women with breast cancer who were treated with multimodal therapies from two institutions were analyzed. We categorized regional nodal irradiation (RNI) as limited RNI, which excluded level I/II, vs extensive RNI, which included level I/II. The ALTJ was delineated retrospectively, and dosimetric and clinical parameters were analyzed to determine the accuracy of predicting the development of lymphedema. Decision tree and random forest algorithms were used to construct the prediction models of the obtained dataset. We used Harrell's C-index to assess discrimination.
Results: The median follow-up time was 77.3 months, and the 5-year lymphedema rate was 6.8 %. According to the decision tree analysis, the lowest lymphedema rate (5-year, 1.2 %) was observed in patients with ≤ six removed lymph nodes and ≤ 66 % ALTJ V35Gy. The highest lymphedema rate was observed in patients with > 15 removed lymph nodes and an ALTJ maximum dose (Dmax) of > 53 Gy (5-year, 71.4 %). Patients with > 15 removed lymph nodes and an ALTJ Dmax ≤ 53 Gy had the second highest rate (5-year, 21.5 %). All other patients had relatively minor differences, with a rate of 9.5 % at 5 years. Random forest analysis revealed that the model's C-index increased from 0.84 to 0.90 if dosimetric parameters were included instead of RNI (P <.001).
Conclusion: The prognostic value of ALTJ for lymphedema was externally validated. The estimation of lymphedema risk based on individual dose-distribution parameters of the ALTJ seemed more reliable than that based on the conventional RNI field design.
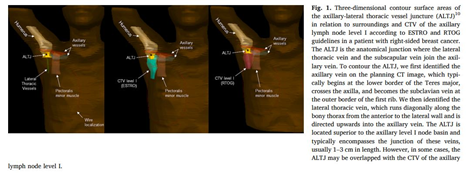
그림. ALTJ is the anatomical junction where the lateral thoracic vein and the subscapular vein join the axillary vein.

그림. Prediction model and a regression tree for predicting 5-year lymphedema risk.
Affiliations
Jee Suk Chang 1, Heejoo Ko 2, Sang Hee Im 3, Jin Sung Kim 1, Hwa Kyung Byun 1, Yong Bae Kim 1, Wonguen Jung 4, Goeun Park 5, Hye Sun Lee 5, Wonmo Sung 6, Robert Olson 7, Chae-Seon Hong 1, Kyubo Kim 4
1Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Republic of Korea.
2College of Medicine, The Catholic University of Korea, Republic of Korea.
3Department and Research Institute of Rehabilitation Medicine, Severance Hospital, Yonsei University College of Medicine, Republic of Korea.
4Department of Radiation Oncology, Ewha Womans University College of Medicine, Republic of Korea.
5Biostatistics Collaboration Unit, Yonsei University College of Medicine, Republic of Korea.
6Department of Biomedical Engineering and of Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
7British Columbia Cancer Agency - Centre for the North, Prince George, BC, Canada.
- 키워드
- ALTJ; Breast cancer; Dose-volume histogram; Lymphedema.
- 연구소개
- 유방암 치료 후 림프부종은 다양한 요인에 의해 발생하며, 최근 방사선치료와 관련한 인자로 ALTJ (axillary-lateral thoracic vessel junture) 선량이 제시된 바 있다. 신촌세브란스병원과 이대목동병원에서 유방암으로 방사선치료를 받은 1449명의 환자를 대상으로 후향적으로 ALTJ를 그려 획득한 dosimetric parameter와 절제된 림프절의 개수 등의 임상정보를 이용하여 림프부종 발생을 예측하는 모델을 구축하였다. 16개 이상의 림프절이 절제되었을 때 ALTJ Vmax가 53 Gy를 넘을 경우 5년 림프부종 발생률은 71.4%, 53 Gy 이하일 경우는 21.5%로 예측되었다. 영역림프절의 범위를 axillary lymph node level에 따라 limited와 extensive 등으로 구분하는 것보다, 개별 환자의 ALTJ 선량을 이용하는 것이 림프부종의 발생률을 보다 정확하게 예측할 수 있을 것으로 기대된다.
- 덧글달기










편집위원
유방암의 수술후 방사선치료 시 주요한 합병증인 림프부종의 예측인자로서 axillary-lateral thoracic vessel juncture (ALTJ)의 dose-effect relationship을 조사한 연구임
2023-06-02 11:29:03
편집위원2
유방암환자에서 axillary-lateral thoracic vessel juncture 부위의 조사선량과 lymphedema 사이의 연관성을 보여주는 연구로 방사선치료 후 lymphedema 발생 위험성을 예측할 수 있는 좋은 수단으로 생각됩니다.
2023-06-09 09:06:51