글로벌 연구동향
방사선종양학
- [In Vivo .] Clinicopathological Outcomes in Patients With Locally Advanced Rectal Cancer Undergoing Preoperative Short- Versus Long-course Chemoradiotherapy With Delayed Surgery
경희대강동병원 / 김재식, 정원규*
- 출처
- In Vivo .
- 등재일
- 2023 Nov-Dec
- 저널이슈번호
- 37(6):2768-2775. doi: 10.21873/invivo.13388.
- 내용
Abstract
Background/aim: We aimed to compare the clinicopathological outcomes in patients with locally advanced rectal cancer after short- or long-course concurrent chemoradiotherapy (CCRT) followed by delayed surgery.Patients and methods: The records of 94 patients with cT3-4N0-2M0 rectal cancer who received CCRT between 2010 and 2017 were reviewed. Short-course radiotherapy (RT) was delivered with a median total dose of 25 Gy in five fractions (n=27), and long-course RT was delivered with a median total dose of 50.4 Gy in 28 fractions (n=67). The following concurrent chemotherapy regimens were administered: 5-fluorouracil plus leucovorin in 58 and capecitabine in 24; in 12 cases agents were unknown. The median interval between CCRT and surgery was 8 weeks. Adjuvant chemotherapy was administered after surgery in 80 patients (5-fluorouracil plus leucovorin, n=54; capecitabine, n=9; other, n=14; and unknown, n=3). Propensity-score matching analysis was conducted.
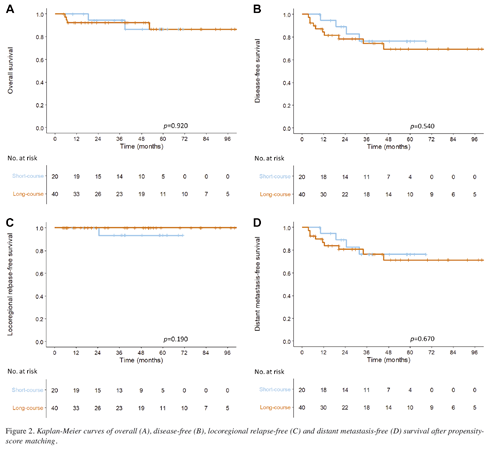
Results: The median follow-up duration was 4.3 years. There were no statistically significant differences between the short- and long-course RT groups in sphincter preservation (85.2% vs. 92.5%, p=0.478), pathological complete remission (18.5% vs. 14.9%, p=0.905), downstaging (44.4% vs. 26.9%, p=0.159), and negative circumferential resection margin (92.6% vs. 89.6%, p=0.947) rates. No differences were found in survival outcomes between the short- and long-course groups at 3 years (overall survival: 91.8% vs. 88.1%, p=0.790; disease-free survival, 75.2% vs. 72.5%, p=0.420; locoregional relapse-free survival, 90.5% vs. 98.4%, p=0.180; and distant metastasis-free survival, 79.6% vs. 73.5%, p=0.490). Similar results were observed after PSM.
Conclusion: Clinically, short-course CCRT may be a feasible alternative to long-course CCRT in patients with locally advanced rectal cancer.
Affiliations
Jae Sik Kim 1 2, Mi Joo Chung 3, Doo Yeul Lee 1, Suk Hwan Lee 4, Seung-Kyu Jeong 5, Byung Eun Yoo 6, Choon Sik Chung 7, Weon Kuu Chung 8
1Department of Radiation Oncology, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea.
2Department of Radiation Oncology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Republic of Korea.
3Department of Radiation Oncology, Hanyang University Changwon Hanmaeum Hospital, Changwon, Republic of Korea.
4Department of Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea.
5Department of Surgery, Yang Hospital, Seoul, Republic of Korea.
6Department of Surgery, Yang Hospital, Namyangju, Republic of Korea.
7Department of Surgery, Hansol Hospital, Seoul, Republic of Korea.
8Department of Radiation Oncology, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea; wkchung16@gmail.com.
- 키워드
- Delayed surgery; preoperative treatment; rectal cancer; short-course chemoradiotherapy.
- 연구소개
- 본 논문에서는 국소 진행 직장암 환자에서 수술 전 단기 혹은 장기 동시 항암화학방사선요법의 치료 성적을 비교한 연구로, 양 군 간에 항문괄약근 보존율, 병리학적 완전 관해율, 종양의 병기 하향율, 측방절제연 음성율에 차이가 없음을 증명하였다. 또한, 치료 성적인 전체 생존율, 무병생존율, 국소영역무재발생존율, 원격전이무병생존율에도 양군 간에 차이가 없었다. 이를 바탕으로 국소 진행 직장암에서 수술 전 단기 동시 항암화학방사선요법이 장기 치료에 대한 대안이 될 수 있음을 보였다.
- 덧글달기
- 이전글 [Int J Radiat Oncol Biol Phys .] Can Definitive Radiation Therapy Substitute Surgical Resection in Locally Advanced T3 or T4 Sinonasal Squamous Cell Carcinoma?
- 다음글 [Cancer Med .] Active involvement of patients, radiation oncologists, and surgeons in a multidisciplinary team approach: Guiding local therapy in recurrent, metastatic rectal cancer










편집위원
국소 진행성 직장암에서 25 Gy/5회의 short-course 항암방사선치료와 50.4 Gy/28회의 long-course 항암방사선치료의 치료 성적 및 예후를 비교한 연구로, short- vs long-course 항암방사선치료 성적과 예후가 통계적으로 차이가 없었으므로, short-course 항암방사선치료가 대체치료방법(alternative treatment option)으로 고려될 수 있다는 결론을 냄.
2024-01-08 10:20:24