글로벌 연구동향
핵의학
- 2020년 05월호
[Eur J Nucl Med Mol Imaging.] Clinicopathologic risk factors of radioactive iodine therapy based on response assessment in patients with differentiated thyroid cancer: a multicenter retrospective cohort study.갑상선암 I-131치료 반응평가기준에 따른 임상요소 차이인제대해운대백병원 / 권성영, 이상우, 배상균*
- 출처
- Eur J Nucl Med Mol Imaging.
- 등재일
- 2020 Mar
- 저널이슈번호
- 47(3):561-571. doi: 10.1007/s00259-019-04634-8. Epub 2019 Dec 10.
- 내용
Abstract
PURPOSE:
We investigated whether predictive clinicopathologic factors can be affected by different response criteria and how the clinical usefulness of radioactive iodine (RAI) therapy should be evaluated considering variable factors in patients with differentiated thyroid carcinoma (DTC).METHODS:
A total of 1563 patients with DTC who underwent first RAI therapy after total or near total thyroidectomy were retrospectively enrolled from 25 hospitals. Response to therapy was evaluated with two different protocols based on combination of biochemical and imaging studies: (1) serum thyroglobulin (Tg) and neck ultrasonography (US) and (2) serum Tg, neck US, and radioiodine scan. The responses to therapy were classified into excellent and non-excellent or acceptable and non-acceptable to minimize the effect of non-specific imaging findings. We investigated which factors were associated with response to therapy depending on the follow-up protocols as well as response classifications. Multivariate logistic regression analysis was performed to identify factors significantly predicting response to therapy.RESULTS:
The proportion of patients in the excellent response group significantly decreased from 76.5 to 59.6% when radioiodine scan was added to the follow-up protocol (P < 0.001). Preparation method (recombinant human TSH vs. thyroid hormone withdrawal) was a significant factor for excellent response prediction evaluated with radioiodine scan (OR 2.129; 95% CI 1.687-2.685; P < 0.001) but was not for other types of response classifications. Administered RAI activity, which was classified as low (1.11 GBq) or high (3.7 GBq or higher), significantly predicted both excellent and acceptable responses regardless of the follow-up protocol.CONCLUSIONS:
The clinical impact of factors related to response prediction differed depending on the follow-up protocol or classification of response criteria. A high administered activity of RAI was a significant factor predicting a favorable response to therapy regardless of the follow-up protocol or classification of response criteria.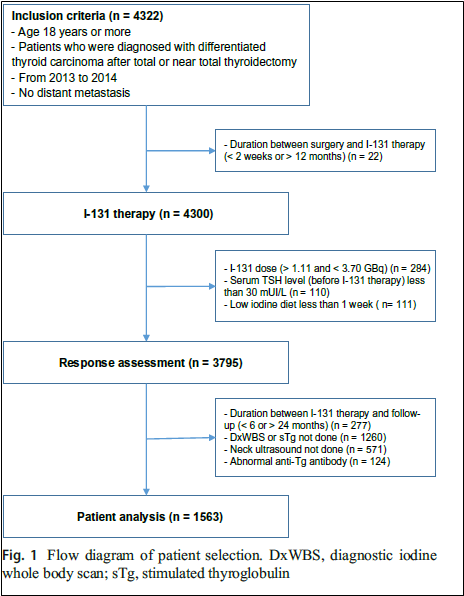
그림 1. 환자 선택 흐름도
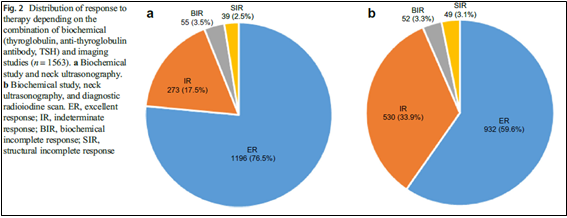
그림 2. 평가기준에 따른 반응의 분포. a. 생화학검사와 목초음파 검사를 이용한 평가결과. b. 생화학검사, 목초음파 검사, 방사성요오드 스캔을 이용한 평가 결과.
Author informationKwon SY1, Lee SW2, Kong EJ3, Kim K4, Kim BI5, Kim J6, Kim H7, Park SH8, Park J9, Park HL10, Oh SW11, Won KS12, Ryu YH13, Yoon JK14, Lee SJ15, Lee JJ16, Chong A17, Jeong YJ18, Jeong JH19, Cho YS20, Cho A21, Cheon GJ22, Choi EK23, Hwang JP24, Bae SK25; Korean Society of Nuclear Medicine (KSNM) Thyroid Cancer Clinical Trial Network (CTN) Retrospective Cohort Study Group.
1
Department of Nuclear Medicine, Chonnam National University Medical School and Hwasun Hospital, Hwasun, Jeonnam, Republic of Korea.
2
Department of Nuclear Medicine, School of Medicine and Chilgok Hospital, Kyungpook National University, Daegu, Republic of Korea.
3
Department of Nuclear Medicine, Yeungnam University Medical School and Hospital, Daegu, Republic of Korea.
4
Department of Nuclear Medicine and Biomedical Research Institute, Pusan National University, Busan, Republic of Korea.
5
Department of Nuclear Medicine, Korea Institute of Radiological & Medical Sciences, Seoul, Republic of Korea.
6
Department of Nuclear Medicine, Chonnam National University Hospital, Gwangju, Republic of Korea.
7
Department of Nuclear Medicine, Kosin University Gospel Hospital, Busan, Republic of Korea.
8
Department of Nuclear Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea.
9
Department of Nuclear Medicine, Inje University Busan Paik Hospital, Busan, Republic of Korea.
10
Division of Nuclear Medicine, Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
11
Department of Nuclear Medicine, Seoul National University Boramae Medical Center, Seoul, Republic of Korea.
12
Department of Nuclear Medicine, Keimyung University Dongsan Hospital, Daegu, Republic of Korea.
13
Department of Nuclear Medicine, Yonsei University Gangnam Severance Hospital, Seoul, Republic of Korea.
14
Department of Nuclear Medicine and Molecular Imaging, Ajou University School of Medicine, Suwon, Republic of Korea.
15
Department of Nuclear Medicine, Hanyang University Medical Center, Seoul, Republic of Korea.
16
Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea.
17
Department of Nuclear Medicine, Chosun University Hospital, Gwangju, Republic of Korea.
18
Department of Nuclear Medicine, Dong-A University Hospital, Busan, Republic of Korea.
19
Department of Nuclear Medicine, Kyungpook National University Hospital, Daegu, Republic of Korea.
20
Department of Nuclear Medicine, Samsung Medical Center, Seoul, Republic of Korea.
21
Department of Nuclear Medicine, Yonsei University College of Medicine, Seoul, Republic of Korea.
22
Department of Nuclear Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea.
23
Division of Nuclear Medicine, Department of Radiology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea.
24
Department of Nuclear Medicine, Soon Chun Hyang University Bucheon Hospital, Bucheon, Republic of Korea.
25
Department of Nuclear Medicine, Inje University Haeundae Paik Hospital, Busan, Republic of Korea. sbae@inje.ac.kr.
- 키워드
- Differentiated thyroid carcinoma; Radioactive iodine therapy; Recombinant human thyrotropin; Response to therapy
- 연구소개
- 2015년 미국갑상선학회(ATA)에서 갑상선암 환자를 위한 진료 가이드라인이 나온 후 우리나라의 진료 환경과는 많이 다른 점이 있었지만 이를 학문적 근거를 가지고 논의할 우리나라만의 자료, 특히 핵의학 분야의 자료가 부족하다고 느끼게 되었습니다. 갑상선암의 방사성요오드 치료에 대한 대한핵의학회 회원들의 의견을 모을 CTN(clinical trial network) 필요성이 대두되어 CTN을 만들고 연구자들을 모았고 당시 대한핵의학회 갑상선연구회 회장을 맡고 있던 제가 주관하게 되었습니다. 25개 기관에서 참여하여 병원당 1-200명의 자료를 수집하여 분석하였고 일차적으로 이 논문을 작성하게 되었습니다. 이 논문에서는 갑상선암에 대한 방사성요오드 치료 평가가 평가기준에 따라 영향을 받는지와 어떻게 방사성요오드 치료의 임상 유용성을 여러 변수 요인을 고려하여 평가해야만 하는지를 조사하였습니다. 결론적으로 반응 예측과 관련된 요인의 임상적 영향은 추적 프로토콜 또는 반응 기준의 분류에 따라 달랐습니다. 고용량의 방사성요오드는 추적 프로토콜 또는 반응 기준의 분류와 무관하게 치료에 대한 좋은 반응을 예측하는 중요한 인자였습니다.
- 덧글달기








편집위원
갑상선암에 대해 다기관 코흐트 연구를 시도한 점과 향후 추가적인 연구주제 발굴의 기초 자료가 될 것으로 생각됩니다.
덧글달기닫기2020-04-27 16:50:34
등록
편집위원2
분화갑상선암에서 방사성요오드치료시 양호한 결과를 나타나게 하는데 어떠한 인자가 있는지를 검토한 다기관 연구임. 해당 연구은 결과에서는 방사성요오드 용량이 높아지면 더 좋은 예후를 보여 준다는 것을 확인하게 하였음. 갑상선암 관련 연구자, 방사성요오드 치료 핵의학의사에게 관심을 끌 논문으로 생각됨.
덧글달기닫기2020-04-27 16:51:10
등록