(구)글로벌 핫이슈
방사선종양학
- [Lancet Oncol.] Radiotherapy in the setting of breast reconstruction: types, techniques, and timing.
Cedars-Sinai Medical Center / Alice Y Ho*
- 출처
- Lancet Oncol.
- 등재일
- 2017 Dec
- 저널이슈번호
- 18(12):e742-e753
- 내용
Abstract
As the use of breast reconstruction and postmastectomy radiotherapy (PMRT) has increased over the past decade, the typical approach to integrating radiotherapy with breast reconstruction has provoked intense controversy in the management of breast cancer. PMRT can lead to an increased frequency of complications in the reconstructed breast. Conversely, the reconstructed breast can increase the complexity of radiotherapy delivery. How to minimise the frequency of complications without compromising oncological or cosmetic outcomes of the reconstructed breast is an important shared multidisciplinary goal for oncologists and their patients. Several questions remain, however, regarding the type of reconstruction that should be used with PMRT, when reconstruction should be done relative to PMRT and whether radiotherapy treatment should be directed towards the tissue expander or the implant for women who opt for a two-stage expander-implant reconstruction. Following advances in the planning of radiotherapy treatment, new questions about the application of these technologies in the setting of breast reconstruction have arisen. In this Review, we address these questions by reviewing contemporary evidence on the optimal integration of radiotherapy and breast reconstruction in the management of breast cancer.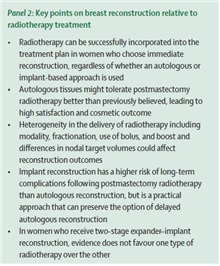
Panel 2: Key points on breast reconstruction relative to radiotherapy treatment
• Radiotherapy can be successfully incorporated into the treatment plan in women who choose immediate reconstruction, regardless of whether an autologous or implant-based approach is used
• Autologous tissues might tolerate postmastectomy radiotherapy better than previously believed, leading to high satisfaction and cosmetic outcome
• Heterogeneity in the delivery of radiotherapy including modality, fractionation, use of bolus, and boost and differences in nodal target volumes could affect reconstruction outcomes
• Implant reconstruction has a higher risk of long-term complications following postmastectomy radiotherapy than autologous reconstruction, but is a practical approach that can preserve the option of delayed autologous reconstruction
• In women who receive two-stage expander–implant reconstruction, evidence does not favour one type of radiotherapy over the otherAuthor information
1
Department of Radiation Oncology, Cedars-Sinai Medical Center, Los Angeles, CA, USA. Electronic address: alice.ho@cshs.org.
2
Icahn School of Medicine, Mount Sinai Health System, New York, NY, USA.
3
Division of Plastic and Reconstructive Surgery, Memorial Sloan Kettering Cancer Center, New York, NY, USA.
4
Section of Plastic Surgery, University of Michigan, Ann Arbor, MI, USA.
- 덧글달기
- 이전글 [Lancet Oncol] Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial.
- 다음글 [J Natl Cancer Inst.] Tumor Regression Grading After Preoperative Chemoradiotherapy as a Prognostic Factor and Individual-Level Surrogate for Disease-Free Survival in Rectal Cancer.










편집위원2
유방전절제술 후 방사선치료를 시행해야 할 때 유방재건술을 언제 하는 것이 부작용이 적으면서 효과적인 미용효과를 얻을 수 있는지 논란이 있는데, 본 리뷰논문을 통해 유방재건술의 방법 및 시기에 따라 적절한 방사선치료를 적용하는데 도움을 받을 수 있겠습니다.
2018-01-10 13:52:26
편집위원
최근 유방재건술 시행이 증가함에 따라 각 기관 별로 다양한 재건방법이 적용되고 있는데, 각각의 장단점 및 방사선치료 시 고려해야 하는 사항에 대해 잘 요약한 리뷰입니다.
2018-01-10 13:42:53