글로벌 연구동향
방사선생물학
- [Anticancer Res.] 직장암에서의 방사선항암치료 예후인자 규명 Predicting Pathological Complete Regression with Haematological Markers During Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer.
서울의대 / 이주호, 김재성*
- 출처
- Anticancer Res.
- 등재일
- 2018 Dec
- 저널이슈번호
- 38(12):6905-6910. doi: 10.21873/anticanres.13067.
- 내용
Abstract
BACKGROUND:
This study evaluated the efficacy of haematological markers for predicting the pathological complete regression (pCR) during and after neoadjuvant chemoradiotherapy (CRT) in patients with locally advanced rectal cancer (LARC).PATIENTS AND METHODS:
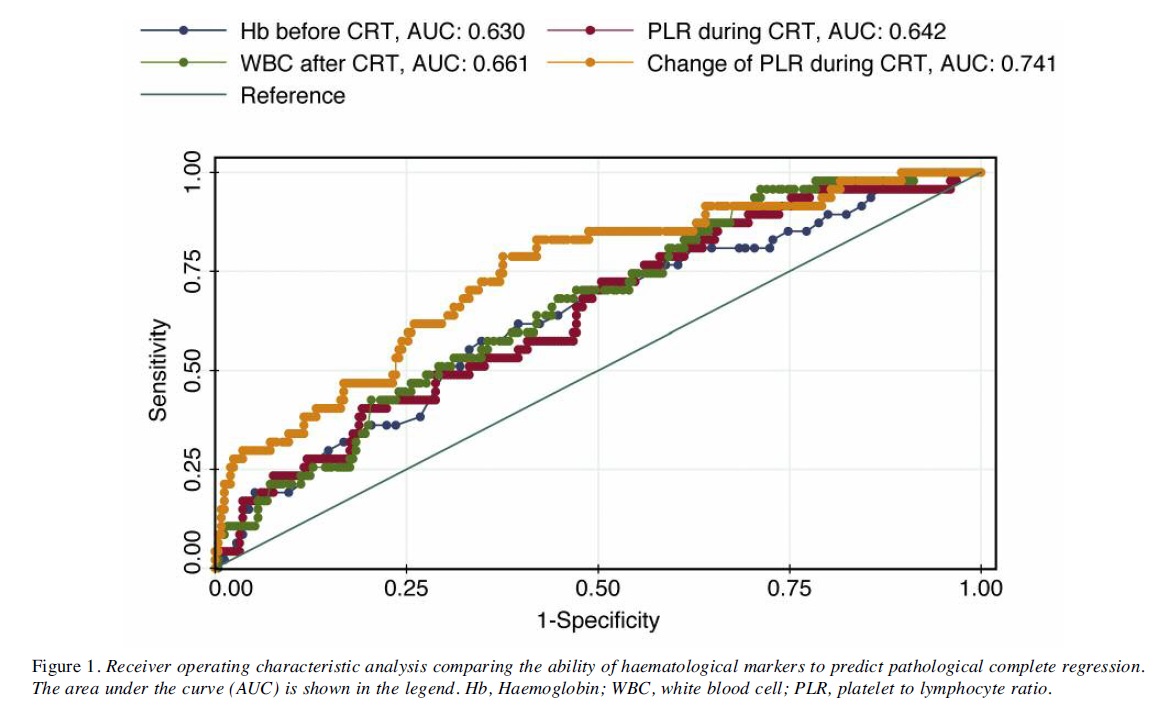
A total of 297 patients with LARC underwent neoadjuvant CRT followed by surgical resection. Complete blood counts (CBCs) were performed before CRT, 3 weeks after the start of CRT (intra-therapy), and 4 weeks after CRT. Platelet-to-lymphocyte ratio (PLR) and neutrophil-to-lymphocyte ratio (NLR) were calculated using the serial CBC test. The ratio of change in PLR (cPLR) and NLR (cNLR) was calculated as the increase from the pre-therapy value to intra-therapy or post-therapy value divided by the pre-therapy value. Chi-square and t-test for univariate analysis and multivariate logistic regression were performed to identify significant predictors for pCR. Receiver operating characteristic (ROC) analysis was used to compare predictive values.RESULTS:
The overall rate of pCR was 15.9%. Pre-therapy high haemoglobin and low NLR; intra-therapy high PLR, high NLR, high cPLR, and high cNLR; and post-therapy low white blood cell count (WBC), high haemoglobin, and high cPLR were significantly associated with pCR. In multivariate logistic regression, pre-therapy high haemoglobin [odds ratio (OR)=1.500, p=0.016], high intra-therapy PLR (OR=1.006, p=0.011), high intra-therapy cPLR (OR=4.948, p<0.001), and low post-therapy WBC (OR=0.639, p=0.003) were significant predictors for pCR. ROC analysis showed that high intra-therapy cPLR was the most accurate predictor of pCR (area under the curve=0.741).CONCLUSION:
Changes of PLR during neoadjuvant CRT for LARC are significant predictors of pCR.
Author informationLee JH1,2, Song C1, Kang SB3, Lee HS4, Lee KW5, Kim JS6.
1
Department of Radiation Oncology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
2
Department of Radiation Oncology, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Republic of Korea.
3
Department of Surgery, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
4
Department of Pathology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
5
Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
6
Department of Radiation Oncology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea jskim@snubh.org.
- 키워드
- Rectal cancer; chemoradiotherapy; complete regression; haematological markers; platelet/lymphocyte ratio
- 연구소개
- 직장암 환자에서 수술 전 항암방사선치료의 치료 후 pathological complete regression 예측에 있어서 치료 전, 중반, 종료 이후 CBC profile 변화 내용을 비교했습니다. 결과적으로 현재 예측 가능성이 높다고 인정되는 치료 전후의 MRI 또는 PET-CT F/U과 비교해서 치료 전과 중반 change of platelet to lymphocyte ratio (cPLR)가 거의 대등한 예측 결과를 보인다는 결과를 제시하여 임상에서 쉽게 치료결과 예측의 참고 자료로 활용할 수 있는 가능성을 제시했습니다.
- 덧글달기









