글로벌 연구동향
의학물리학
- 2019년 06월호
[Med Phys.] Technical Note: Simplified and practical pretherapy tumor dosimetry - A feasibility study for 131 I-MIBG therapy of neuroblastoma using 124 I-MIBG PET/CT.University of California / 서영호*
- 출처
- Med Phys.
- 등재일
- 2019 May
- 저널이슈번호
- 46(5):2477-2486. doi: 10.1002/mp.13446. Epub 2019 Mar 12.
- 내용
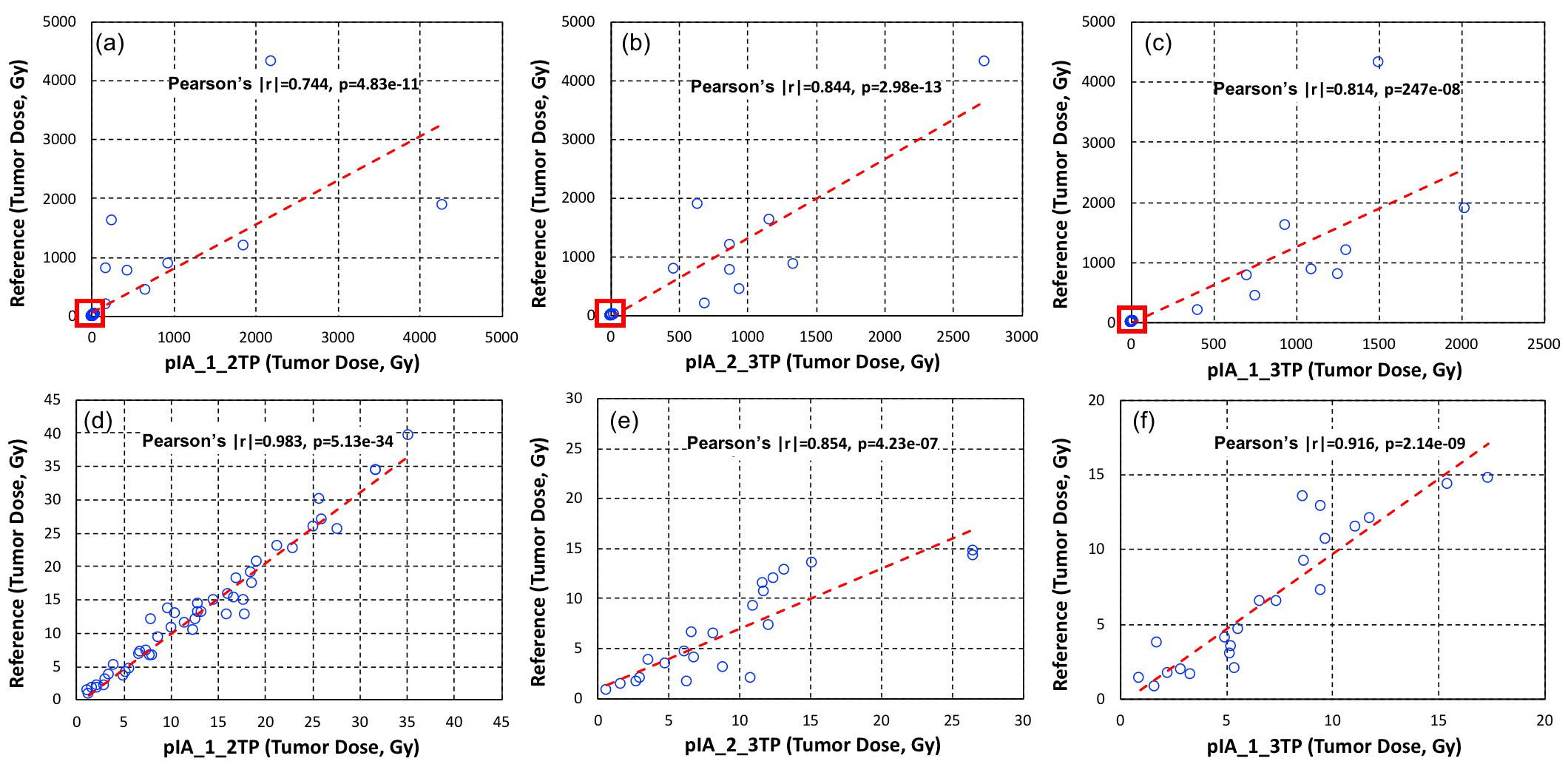
Reference tumor dose (Gy) vs tumor doses calculated using the two‐time points (Gy) with percent of injected activities areas between time point 1 and time point 2 (a, d), time point 2 and time point 3 (b, e), and time point 1 and time point 3 (c, f). The enlarged portions of plots (d, e, f) from the red box in the upper plots (a, b, c) show the difference in calculated doses under 100 Gy.
<Reprinted with permission from John Wiley & Sons, Inc. >
Abstract
PURPOSE:
Radiation dose calculated on tumors for radiopharmaceutical therapy varies significantly from tumor to tumor and from patient to patient. Accurate estimation of radiation dose requires multiple time point measurements using radionuclide imaging modalities such as SPECT or PET. In this report, we show our technical development of reducing the number of scans needed for reasonable estimation of tumor and normal organ dose in our pretherapy imaging and dosimetry platform of 124 I-metaiodobenzylguanidine (MIBG) positron emission tomography/computed tomography (PET/CT) for 131 I-MIBG therapy of neuroblastoma.METHODS:
We analyzed the simplest kinetic data, areas of two-time point data for five patients with neuroblastoma who underwent 3 or 4 times of 124 I-MIBG PET/CT scan prior to 131 I-MIBG therapy. The data for which we derived areas were percent of injected activity (%IA) and standardized uptake value of tumors. These areas were correlated with time-integrated activity coefficients (TIACs) from full data (3 or 4 time points). TIACs are direct correlates with radiation dose as long as the volume and the radionuclide are known.RESULTS:
The areas of %IAs between data obtained from all the two-time points with time points 1 and 2 (day 0 and day 1), time points 2 and 3 (day 1 and day 2), and time points 1 and 3 (day 0 and day 2) showed reasonable correlation (Pearson's correlation coefficient |r| > 0.5) with not only tumor and organ TIACs but also tumor and organ absorbed doses. The tumor and organ doses calculated using %IA areas of time point 1 and time point 2 were our best fits at about 20% individual percent difference compared to doses calculated using 3 or 4 time points.CONCLUSIONS:
We could achieve reasonable accuracy of estimating tumor doses for subsequent radiopharmaceutical therapy using only the two-time point imaging sessions. Images obtained from these time points (within the 48-h after administration of radiopharmaceutical) were also viewed as useful for diagnostic reading. Although our analysis was specific to 124 I-MIBG PET/CT pretherapy imaging data for 131 I-MIBG therapy of neuroblastoma and the number of imaging datasets was not large, this feasible methodology would generally be applicable to other imaging and therapeutic radionuclides with an appropriate data analysis similar to our analysis to other imaging and therapeutic radiopharmaceuticals.
Author informationSeo Y1,2,3,4, Huh Y1, Huang SY1, Hernandez-Pampaloni JM1, Hawkins RA1, Gustafson WC5, Vo KT5, Matthay KK5.
1
Department of Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, USA.
2
Department of Radiation Oncology, University of California, San Francisco, San Francisco, CA, USA.
3
Joint Graduate Group in Bioengineering, University of California, San Francisco, Berkeley, CA, USA.
4
Bakar Computational Health Sciences Institute, University of California, San Francisco, San Francisco, CA, USA.
5
Department of Pediatrics, University of California, San Francisco, San Francisco, CA, USA.
- 키워드
- MIBG ; dosimetry; neuroblastoma; radionuclide therapy; tumor dosimetry
- 연구소개
- 치료 목적으로 쓰여지는 방사성 동위원소 의약품은 환자 맞춤형 방사선량을 구하기가 어려운 걸로 알려져 있습니다. 치료용 방사성 의약품에 사용되는 동위원소와 화학적으로 동일한 정량적인 영상을 얻을 수 있는 동위원소가 있는 경우에 영상을 통해서 방사선량을 구하는 방법이 계속 연구되어 왔지만 영상을 적어도 3번에서 5번을 일주일 정도의 시간에 걸쳐 찍어야 하는 번거로움이 큰 문제로 지적되어 왔습니다. 본 연구에서는 소아암의 일종인 신경모세포종 (neuroblastoma)의 치료에 쓰이는 131I-MIBG의 방사선량을 단 이틀간 2번의 124I-MIBG PET/CT 영상 정보를 이용해서 상당히 정확하게 측정하는 방법을 개발하였습니다. 종양에 부여되는 방사선량뿐 아니라 환자의 안전에 직접적인 영향을 미치는 일반 장기의 방사선량까지 같은 방법으로 구할 수 있음을 보여주었습니다. 비슷한 방법이 다른 치료용 방사성 동위원소 의약품의 환자맞춤 방사선량을 구하는데도 충분히 쓰여질 수 있을거라 예측됩니다.
- 덧글달기








편집위원
본 연구는, 방사성의약품 치료(radiopharmaceutical therapy)에서 치료 시행전 필수적인 내부 방사선량 측정 기술의 실용성 향상을 위한 연구로, 방사선량 측정을 위해 필요한 핵의학영상 횟수를 줄이고 촬영 시점 또한 앞당겨 실용성을 확보하면서도 측정 정확도도 비슷한 수준으로 유지할 수 있는 방법을 소개하였다. 향후 좀 더 많은 데이터와 다른 방사성의약품 데이터를 기반으로 추가적인 검증이 이루어진다면, 실제 치료에 유용하게 사용될 수 있을 것으로 예상된다.
덧글달기닫기2019-06-24 13:52:46
등록