글로벌 연구동향
방사선종양학
- [Radiother Oncol.] Postoperative radiotherapy for WHO grade II-III intracranial ependymoma in adults: An intergroup collaborative study (KROG 18-06/KNOG 18-01)
서울의대 / 위찬우, 김인아*
- 출처
- Radiother Oncol.
- 등재일
- 2020 Jun 2
- 저널이슈번호
- 150:4-11. doi: 10.1016/j.radonc.2020.05.045. Online ahead of print.
- 내용
Abstract
Background and purpose: To evaluate the impact of adjuvant postoperative radiotherapy (PORT) in adult WHO grade II-III intracranial ependymoma (IEPN).Materials and methods: A total of 172 pathologically confirmed adult grade II-III IEPN patients from 12 institutions were eligible. Of them, 106 (61.6%) and 66 (38.4%) patients were grade II and III, respectively. For grade II and III IEPNs, 51 (48.1%) and 59 (89.4%) patients received PORT, respectively. The median dose to the primary tumor bed was 54.0 Gy and 59.4 Gy for grade II and III patients, respectively. The prognostic impact of sex, age, performance, WHO grade, location, size, surgical extent, and PORT on local control (LC), progression-free survival (PFS), and overall survival (OS) were evaluated by univariate and multivariate analysis.
Results: The median follow-up period for survivors was 88.1 months. The 5-/10-year LC, PFS, and OS rates were 64.8%/54.0%, 56.4%/44.8%, and 76.6%/71.0%, respectively. On multivariate analysis, adjuvant PORT significantly improved LC (P = 0.002), PFS (P = 0.002), and OS (P = 0.043). Older age (P < 0.001), WHO grade III (P < 0.001), larger tumor size (P = 0.004), and lesser surgical extent (P < 0.001) were also negative factors for OS. Adjuvant PORT also improved LC (P = 0.010), PFS (P = 0.007), and OS (P = 0.069) on multivariate analysis for grade II IEPNs.
Conclusion: This multicenter retrospective study supports the role of adjuvant PORT in terms of disease control and survival in adult grade II-III IEPNs. Prospective randomized trials focused on individualized treatment based on molecular subtypes is warranted.
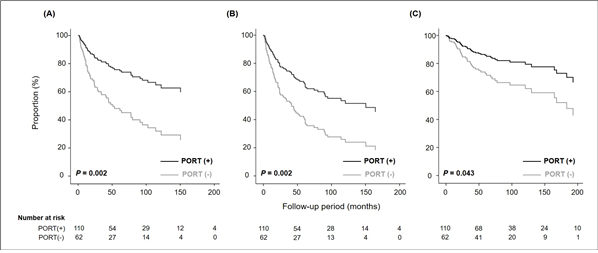
Figure 1. Adjusted survival curves using the Cox proportional hazard model for (A) local control, (B) progression-free survival, and (C) overall survival based on the use of postoperative radiotherapy in WHO grade II–III patients.
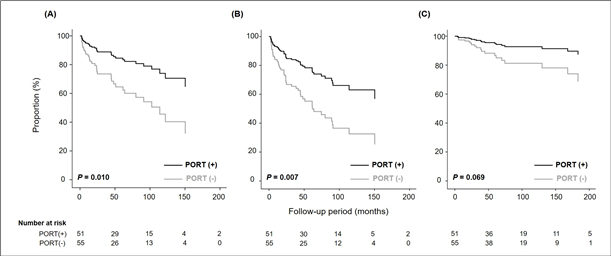
Figure 2. Adjusted survival curves using the Cox proportional hazard model for (A) local control, (B) progression-free survival, and (C) overall survival based on the use of postoperative radiotherapy in WHO grade II patients.
AffiliationsChan Woo Wee 1 , Il Han Kim 2 , Chul-Kee Park 3 , Do Hoon Lim 4 , Do-Hyun Nam 5 , Hong In Yoon 6 , Chang-Ok Suh 6 , Jong Hee Chang 7 , Woong-Ki Chung 8 , Tae-Young Jung 9 , Shin-Hyung Park 10 , Chae-Yong Kim 11 , Young Zoon Kim 12 , Ho Shin Gwak 13 , Kwan Ho Cho 14 , Jin Hee Kim 15 , Jung Ho Im 16 , Woo Chul Kim 17 , Sung-Hwan Kim 18 , In Ah Kim 19
1 Department of Radiation Oncology, SMG-SNU Boramae Medical Center, Seoul, Republic of Korea.
2 Department of Radiation Oncology, Seoul National University Hospital, Republic of Korea.
3 Department of Neurosurgery, Seoul National University Hospital, Republic of Korea.
4 Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea.
5 Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea.
6 Department of Radiation Oncology, Yonsei Cancer Center, Seoul, Republic of Korea.
7 Department of Neurosurgery, Yonsei Cancer Center, Seoul, Republic of Korea.
8 Department of Radiation Oncology, Chonnam National University Hwasun Hospital, Hwasun, Republic of Korea.
9 Department of Neurosurgery, Chonnam National University Hwasun Hospital, Hwasun, Republic of Korea.
10 Department of Radiation Oncology, School of Medicine, Kyungpook National University, Daegu, Republic of Korea.
11 Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Republic of Korea.
12 Division of Neuro-Oncology and Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Republic of Korea.
13 Department of Neurosurgery, National Cancer Center, Goyang, Republic of Korea.
14 Proton Therapy Center, National Cancer Center, Goyang, Republic of Korea.
15 Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Daegu, Republic of Korea.
16 Department of Radiation Oncology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Republic of Korea.
17 Department of Radiation Oncology, Inha University Hospital, Incheon, Republic of Korea.
18 Department of Radiation Oncology, St. Vincent's Hospital, Suwon, Republic of Korea.
19 Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Republic of Korea. Electronic address: inah228@snu.ac.kr.
- 연구소개
- 성인 두개골내 상의세포종은 성인 뇌종양의 약 1–2%를 차지하는 매우 드문 종양으로 수술 후 방사선치료의 효용성이 3상 무작위 임상시험을 통해 입증된 바가 없다. 이에 대한방사선종양학회와 대한신경종양학회가 협력하여 다기관 연구를 수행하였다. 수술을 통해 조직학적으로 WHO II–III 등급의 상의세포종으로 확진된 172명의 성인들에서 수술과 수술+방사선치료의 성적을 비교하였다. 88개월간의 추적관찰 결과 전체 환자들의 5년 국소조절율, 무진행생존율, 전체생존율은 각각 65%, 56%, 77%였다. 단변량 분석결과 수술 후 방사선치료는 국소조절율, 무진행생존율, 전체생존율을 향상시키지 못하는 것으로 나타났으나 수술 군과 수술+방사선치료 군 간에는 가장 중요한 예후인자인 절제범위의 유의한 차이 (P=0.013)를 보였다. 이와 다른 인자들을 보정하여 다변량 Cox regression analysis를 시행하였을때는 수술 후 방사선치료가 국소조절율 (P=0.002), 무진행생존율 (P=0.002), 전체생존율 (P=0.043) 모두를 유의하게 향상시키는 결과를 보여주었다 (Figure 1). 방사선치료여부에 가장 논란이 있는 II등급 상의세포종만을 대상으로 다변량 분석을 하였을때도 방사선치료는 국소조절율 (P=0.010), 무진행생존율 (P=0.007), 전체생존율 (P=0.069)을 향상시켰다 (Figure 2). 본 연구는 현재까지 성인 두개골내 상의세포종 환자들의 치료에 있어 방사선치료의 효용성을 입증한 가장 큰 규모의 연구 중 하나로 임상적인 가치가 크다고 볼 수 있겠다. 다시 한번 연구에 많은 도움을 주신 국내의 방사선종양학과와 신경외과 선생님들께 감사를 표합니다.
- 덧글달기
- 이전글 [Cancer Res Treat.] Clinical Outcomes of Immune Checkpoint Blocker Therapy for Malignant Melanoma in Korean Patients: Potential Clinical Implications for a Combination Strategy Involving Radiotherapy
- 다음글 [J Breast Cancer] Impact of Oncotype DX Recurrence Score on the Patterns of Locoregional Recurrence in Breast Cancer (Korean Radiation Oncology Group 19-06)









