글로벌 연구동향
방사선종양학
- 2020년 07월호
[Radiother Oncol.] Comparison of Clinical Outcomes Between Passive Scattering Versus Pencil-Beam Scanning Proton Beam Therapy for Hepatocellular Carcinoma성균관의대 / 유규상, 유정일, 박희철*
- 출처
- Radiother Oncol.
- 등재일
- 2020 May
- 저널이슈번호
- 146:187-193. doi: 10.1016/j.radonc.2020.02.019. Epub 2020 Mar 14.
- 내용
Abstract
Background and purpose: Our study aimed to compare the oncologic outcomes and toxicities between passive scattering (PS) proton beam therapy (PBT) and pencil-beam scanning (PBS) PBT for primary hepatocellular carcinoma (HCC).Materials and methods: The multidisciplinary team for liver cancer identified the PBT candidates who were ineligible for resection or radiofrequency ablation. We retrospectively analyzed 172 patients who received PBT for primary HCC from January 2016 to December 2017. The PS with wobbling method was applied with both breath-hold and regular breathing techniques, while the PBS method was utilized only for regular breathing techniques covering the full amplitude of respiration. To maintain the balance of the variables between the PS and PBS groups, we performed propensity score matching.
Results: The median follow-up duration for the total cohort was 14 months (range, 1-31 months). After propensity score matching, a total of 103 patients (70 in the PS group and 33 in the PBS group) were included in analysis. There were no significant differences in the rates of overall survival (OS), in-field local control (IFLC), out-field intrahepatic control (OFIHC), extrahepatic progression-free survival (EHPFS), and complete response (CR) between the matched groups. In the subgroup analyses, no subgroup showed a significant difference in IFLC between the PS and PBS groups. There was also no significant difference in the toxicity profiles between the groups.
Conclusion: There are no differences in oncologic outcomes, including OS, IFLC, OFIHC, EHPFS, and CR rates, or in the toxicity profiles between PS and PBS PBT for primary HCC.
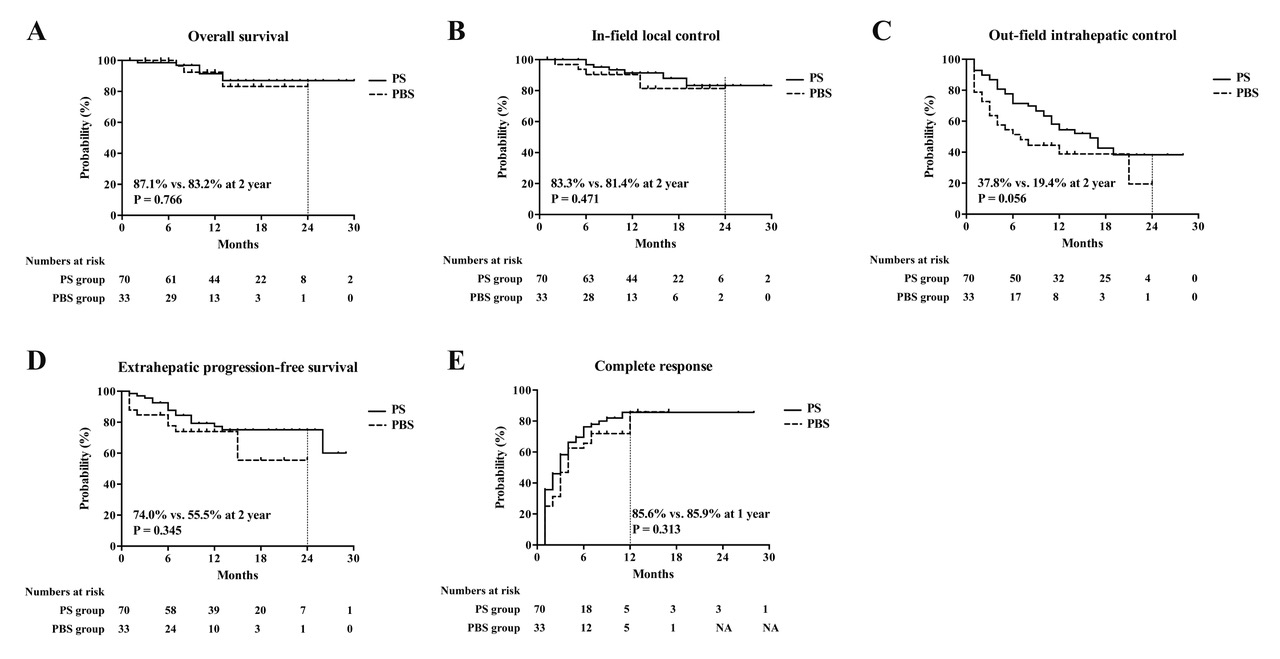
Fig. 1. Kaplan-Meier’s curves for (A) overall survival, (B) in-field local control (C), out-field intrahepatic control, (D) extrahepatic progression-free survival, and (E) complete response.
PS, passive scattering; PBS, pencil-beam scanning
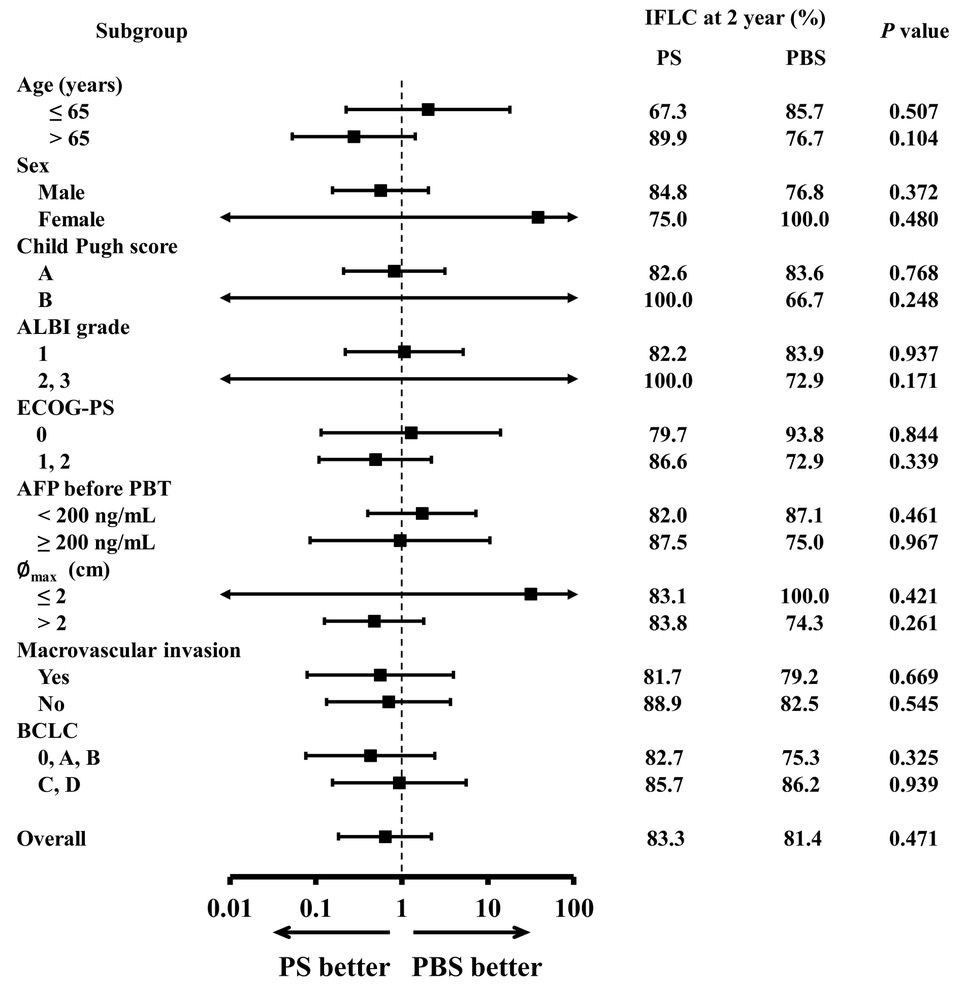
Fig. 2. Subgroup analysis for in-field local control
IFLC, in-field local control; PS, passive scattering; PBS, pencil-beam scanning; ALBI, albumin-bilirubin; ECOG-PS, Eastern Cooperative Oncology Group performance status; AFP, alpha-fetoprotein; PBT, proton beam therapy; Med., median; ∅max, maximum diameter; BCLC, Barcelona Clinic Liver Cancer
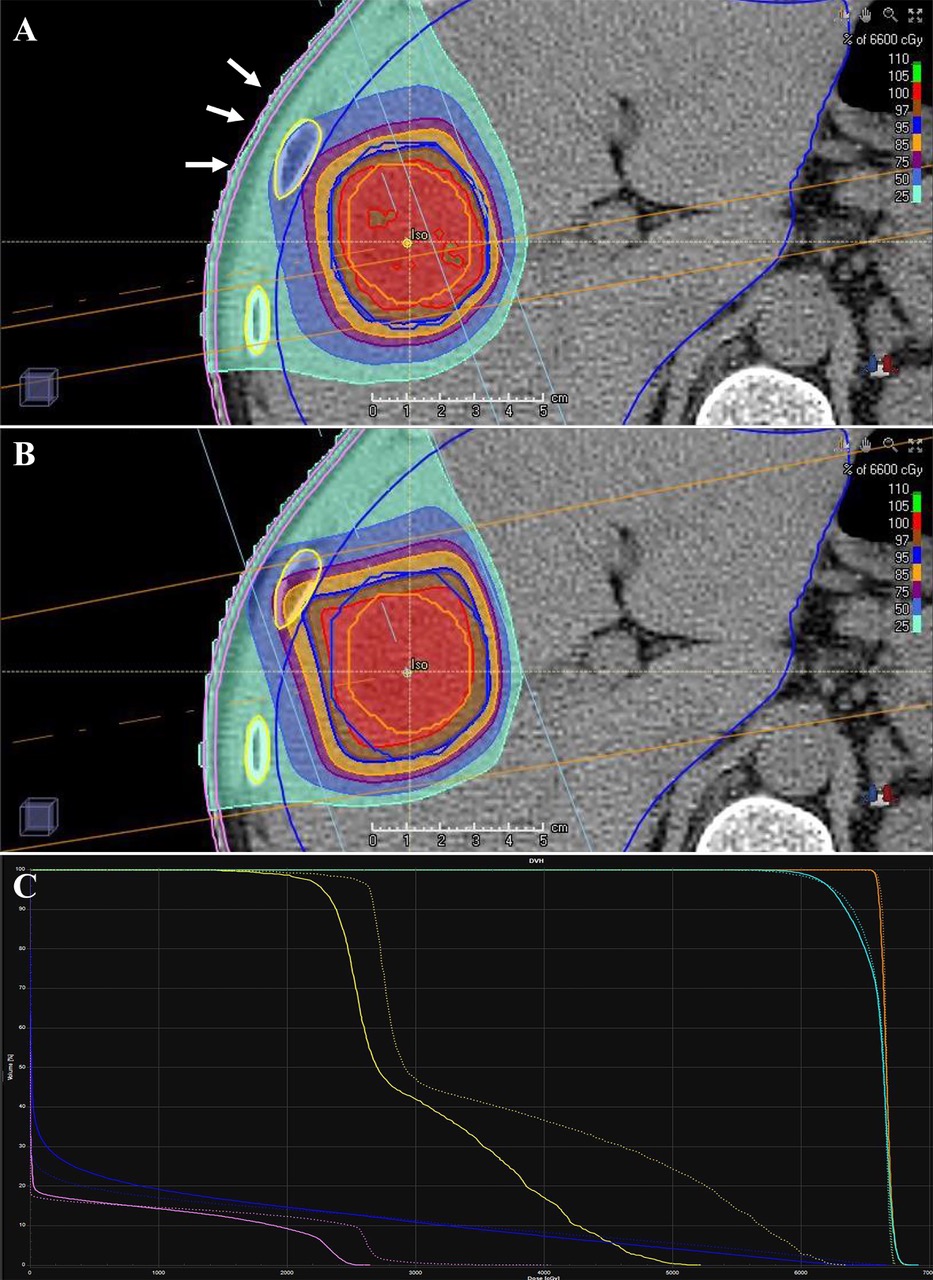
Fig 3. The comparison of dosimetry between pencil-beam scanning (PBS) and passive scattering (PS) proton beam therapy (PBT) of 66 GyRBE in 10 fractions. The PBS (A) shows better conformality than PS PBT (B) along the proximal edge (white arrows). Due to the better conformality, the dose at the chest wall (pink line) and rib (yellow line) are lower in the PBS (solid line) than PS (dotted line) as dose-volume histogram shows (C). The orange, sky blue, and blue lines represent the dose-volume histogram of gross tumor volume, clinical target volume, and normal liver, respectively (C).
Affiliations
Gyu Sang Yoo 1 , Jeong Il Yu 1 , Sungkoo Cho 2 , Sang Hoon Jung 2 , Youngyih Han 1 , Seyjoon Park 2 , Yoonjin Oh 2 , Boram Lee 2 , Hee Chul Park 3 , Do Hoon Lim 1 , Moon Seok Choi 4 , Hojeong Won 5
1 Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea.
2 Department of Radiation Oncology, Samsung Medical Center, Seoul, Republic of Korea.
3 Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea. Electronic address: rophc@skku.edu.
4 Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea.
5 Statistics and Data Center, Research Institute for Future Medicine, Samsung Medical Center, Seoul, Republic of Korea.
- 키워드
- Hepatocellular carcinoma; Local control; Passive scattering; Pencil-beam scanning; Proton beam therapy; Toxicity.
- 연구소개
- 과거 원발 간세포암의 방사선치료는 방사선에 의한 간조직 손상의 우려 등으로 그 이용이 상당히 제한되었으나, 방사선치료 기법의 발달로 그 이용빈도가 증가하고 있다. 최첨단의 방사선치료 기법 중 양성자치료는 출구 선량이 없다는 장점을 갖고 있어 원발 간세포암의 방사선치료에 각광을 받고 있으며 그 동안 치료의 안정성과 효과를 뒷받침하는 많은 임상결과가 보고되어 왔다. 그러나 기존의 보고는 양성자치료 기술 중 수동산란 (passive scattering) 방식을 적용했을 때의 결과인데 반해 현재에는 더 정밀한 선량 조사가 가능한 주사 (scanning) 방식의 노즐 (nozzle) 장착이 대세로 자리잡고 있으며, 아직까지는 주사 방식의 양성자치료를 적용했을 때 원발 간세포암의 치료 성적이 제대로 보고된 바가 없다. 본 연구에서는 원발 간세포암의 양성자치료에 있어서 수동산란 방식과 주사 방식 간의 치료 성적 및 독성을 비교하였다. 양 군의 환자 분포를 균일하게 하기 위해여 성향점수매칭을 적용하였고, 종양의 국소제어율, 종양 반응을 비롯한 종양학적 성적과 간 독성 등의 치료 부작용 빈도에서 양 군간 통계적으로 유의한 차이가 없었다. 또한 다양한 아군 (subgroup)에서 두 치료 기법의 국소제어율를 비교했지만, 국소제어율에 차이를 보이는 아군을 찾지 못하였다. 본 연구는 원발 간세포암 환자에서 두 양성자치료 기법의 치료 성적을 비교한 첫 연구라는 점에서 의의가 있다.
- 덧글달기







